Emergency medical services are an essential part of citizen security. This has prompted the NAOF to audit the functioning of the emergency medical service chain. Concentration of the services in fewer locations, ageing of the population and the need for more services as a result will increase the need for emergency medical services. At the moment, emergency care units must manage a large number of non-urgent tasks that should be carried out in a different manner. Closer cooperation, better information collection and better planning of resources could also help to make emergency medical services more efficient.
In emergency medical services, an acutely ill or injured patient is provided with urgent care and, if necessary, transported to further care. Emergency medical services are based on the cooperation between emergency response centres, emergency care units and outpatient clinics.
The NAOF audited the emergency medical service chain to determine whether it functions properly because emergency medical services are an essential part of citizen security. Concentration of healthcare and social welfare services in fewer locations and more extensive use of home care services have led to an increase in non-urgent emergency care tasks, such as transporting of elderly people to outpatient clinics. Non-urgent transport assignments increase the workload of emergency medical services and take resources from urgent tasks. As a result, those in need of assistance may have to wait for emergency care. Total costs of emergency medical services are estimated at EUR 300 million each year. Hospital districts pay two thirds of this total.
The National Audit Office recommends that new services should be created between emergency medical services and home care so that the number of non-urgent emergency care transport tasks can be reduced. Even though the development of services is already under way, additional services are needed, especially between emergency medical services and home care. Investing in well-functioning home care and introducing the planned support measures would generate savings because compared with them, emergency medical services are expensive.
The number of non-urgent tasks could also be reduced by harmonising the instructions issued by hospital districts to call-takers in emergency response centres. The existing instructions leave room for interpretation and they may prompt call-takers to use emergency medical services in situations where they are not needed. The call-takers use the instructions as a basis when determining the urgency and resource-intensity of the emergency task.
Emergency medical service resources could be used more efficiently if there was a better flow of communications and closer cooperation between emergency medical services, outpatient clinics, social emergency services, home care and home health care. The lack of a joint data resource and a large number of different information systems make the planning of emergency medical service resources more difficult.
Travel cost reimbursement payments by the Social Insurance Institution of Finland account for one third of all emergency medical service costs. They are paid to emergency medical service providers on the basis of distances travelled and the time spent on the assignments and not on the basis of the urgency of the tasks. The system creates unhealthy incentives for the service providers and does not encourage them to use the resources efficiently. Thus, the updating of the system should be completed.
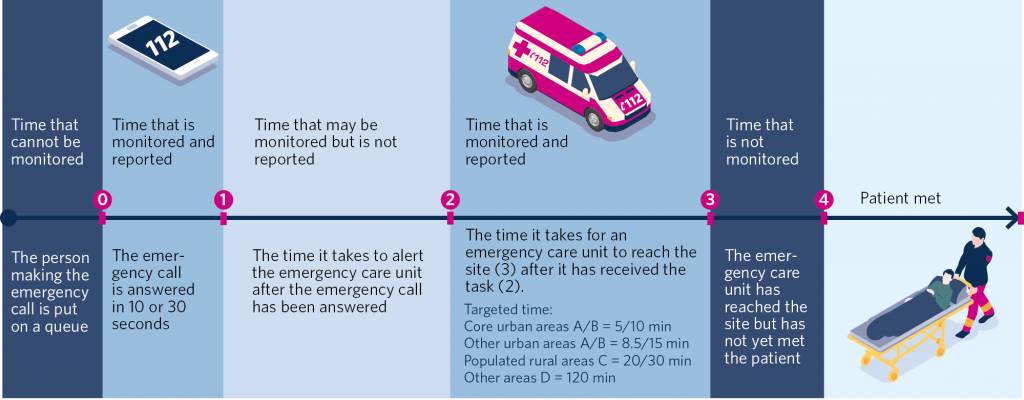
Figure: Stages of the emergency medical service chain and monitoring them
URN identification




